Clinical Nurse Leader: Everything you need to Know
The healthcare landscape is growing increasingly complex due to rapid technological advancements, evolving patient needs, and an aging population. The rise of chronic diseases, digital health solutions, and AI-driven care demands continuous learning and adaptability from professionals. Regulatory challenges, insurance policies, and workforce shortages further strain the system, emphasizing the need for strategic reforms. As healthcare integrates telemedicine and data-driven decision-making, balancing innovation with ethical considerations and patient safety remains crucial. A focus on interdisciplinary collaboration, technology integration, and patient-centered care will be key to ensuring accessible, high-quality healthcare.
Leadership roles in nursing, including that of a Clinical Nurse Leader (CNL), are essential for ensuring high-quality patient care, fostering teamwork, and driving improvements within healthcare systems. Clinical Nurse Leaders not only provide clinical expertise but also inspire, mentor, and advocate for both patients and fellow healthcare professionals. Effective leadership enhances communication, improves decision-making, and promotes a culture of safety and continuous learning. In an increasingly complex healthcare environment, strong nursing leadership, particularly through the role of a Clinical Nurse Leader is crucial for managing resources efficiently, implementing evidence-based practices, and adapting to new challenges. By empowering nurses at all levels, including Clinical Nurse Leaders, to take on leadership roles, healthcare organizations can enhance patient outcomes, improve workplace morale, and drive meaningful change in the profession. The CNL designs, implements, and evaluates patient care by coordinating, delegating, and supervising the healthcare team, including licensed nurses, technicians, and other professionals, ensuring optimal care delivery.
What is a clinical nurse leader?
The Clinical Nurse Leader (CNL) is a master's-prepared nurse equipped to provide care across various healthcare settings in today’s evolving healthcare landscape. The American Association of Colleges of Nursing (AACN), in collaboration with various healthcare organizations and disciplines, introduced the Clinical Nurse Leader (CNL) role in 2003—the first new nursing role in over 35 years—in response to the growing demand for change in the healthcare system. The necessary competencies for CNLs were initially outlined by the AACN Task Force on Education & Regulation II (TFERII) in the Working Paper on the Clinical Nurse Leader. In 2007, the AACN Board of Directors approved the White Paper on the Education and Role of the Clinical Nurse Leader, which provided an in-depth overview of the CNL role, educational framework, expected outcomes, and essential competencies for graduates.
As a leader in healthcare delivery, the CNL plays a vital role in diverse clinical environments, though their specific responsibilities may vary. Unlike administrative or managerial roles, the CNL is directly accountable for patient care outcomes, utilizing evidence-based practices to design, implement, and evaluate care models. Serving as both a provider and coordinator of care, the CNL ensures high-quality patient care at the point of service for individuals and groups across different healthcare settings.
Key aspects of Clinical Nurse Leader (CNL) practice include:
Providing clinical leadership in patient care, including designing, coordinating, and evaluating care for individuals, families, groups, and populations.
Contributing to the identification and collection of care outcomes.
Taking accountability for assessing and improving point-of-care outcomes by synthesizing data and evidence to achieve optimal results.
Anticipating risks for individual patients and patient groups.
Ensuring seamless coordination and integration of care across different healthcare settings.
Designing and implementing evidence-based practices.
Leading, managing, and collaborating with interdisciplinary healthcare teams.
Utilizing information systems and technology to enhance healthcare outcomes.
Managing and optimizing human, environmental, and material resources.
Advocating for patients, communities, and the healthcare team.
Responsibilities of a Clinical Nurse Leader
Leading and coordinating care for patients across various healthcare settings.
Implementing evidence-based practices to improve clinical outcomes.
Identifying and addressing risks to patient safety and care quality.
Advocating for patients and ensuring person-centered care.
Promoting interdisciplinary collaboration among healthcare teams.
Mentoring and educating nursing staff to enhance professional development.
Utilizing data analytics and healthcare informatics to drive decision-making.
Clinical nurse leader competencies
Analyze Data and Benchmarking:
Analyze quantitative and qualitative data to assess care outcomes.
Benchmark outcomes against industry standards.
Communicate trends and outcomes effectively using various media channels.
Promote Social Justice and Equity:
Address healthcare disparities through social, political, economic, and historical factors.
Improve healthcare quality by promoting social justice.
Utilize Improvement Science and Systems Theory:
Apply improvement science and systems theory to enhance care delivery.
Understand healthcare systems, including delivery models, payment structures, and the roles of healthcare professionals, patients, and caregivers.
Lead interprofessional teams focused on patient-centered care and cost-effective quality improvement.
Use systems theory to assess, design, and evaluate healthcare delivery in complex organizations.
Business and Economic Knowledge:
Demonstrate knowledge of budgeting, strategic planning, and value-based purchasing.
Contribute to microsystem-level budget development.
Evaluate evidence-based care delivery approaches.
Collaborate with healthcare professionals to plan, implement, and evaluate improvement initiatives.
Continuous Quality Improvement:
Foster a culture of continuous quality improvement using evidence, analytics, and safety tools (e.g., FMEA, RCA) to reduce risks.
Assess patient handoffs and transitions of care, medication reconciliation, and administration processes.
Present business plans and use diverse datasets like HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) to assess health risks and outcomes.
Collaboration and Ethical Decision-Making:
Collaborate with healthcare teams to apply evidence-based practices.
Promote a culture of inquiry and ensure ethical decision-making.
Use performance measures to guide change initiatives and share practice changes with stakeholders.
Integrate technologies to improve patient care coordination.
Advocate for Wellness and Cost-Effective Care:
Advocate for policies that promote wellness and improve care outcomes.
Support cost-effective care and value-based purchasing.
Promote the Role of Clinical Nurse Leader (CNL):
Promote the CNL role as a leader within interprofessional teams.
Support collaborative care approaches to enhance patient outcomes.
Guide team decisions using tools like SWOT, Pareto, and brainstorming.
Drive care transitions to reduce recidivism.
Engage with Community and Social Service Systems:
Engage with community and social service systems to design patient-centered, culturally appropriate health services.
Assess emergency preparedness and incorporate public health concepts into preventive services.
Effective Communication and Leadership:
Communicate effectively across verbal, non-verbal, written, and virtual formats.
Coach, delegate, and ensure safe, competent care delivery.
Advocate for patients and develop community partnerships.
Ensure care for at-risk populations and assist in quality-of-life and end-of-life decisions.
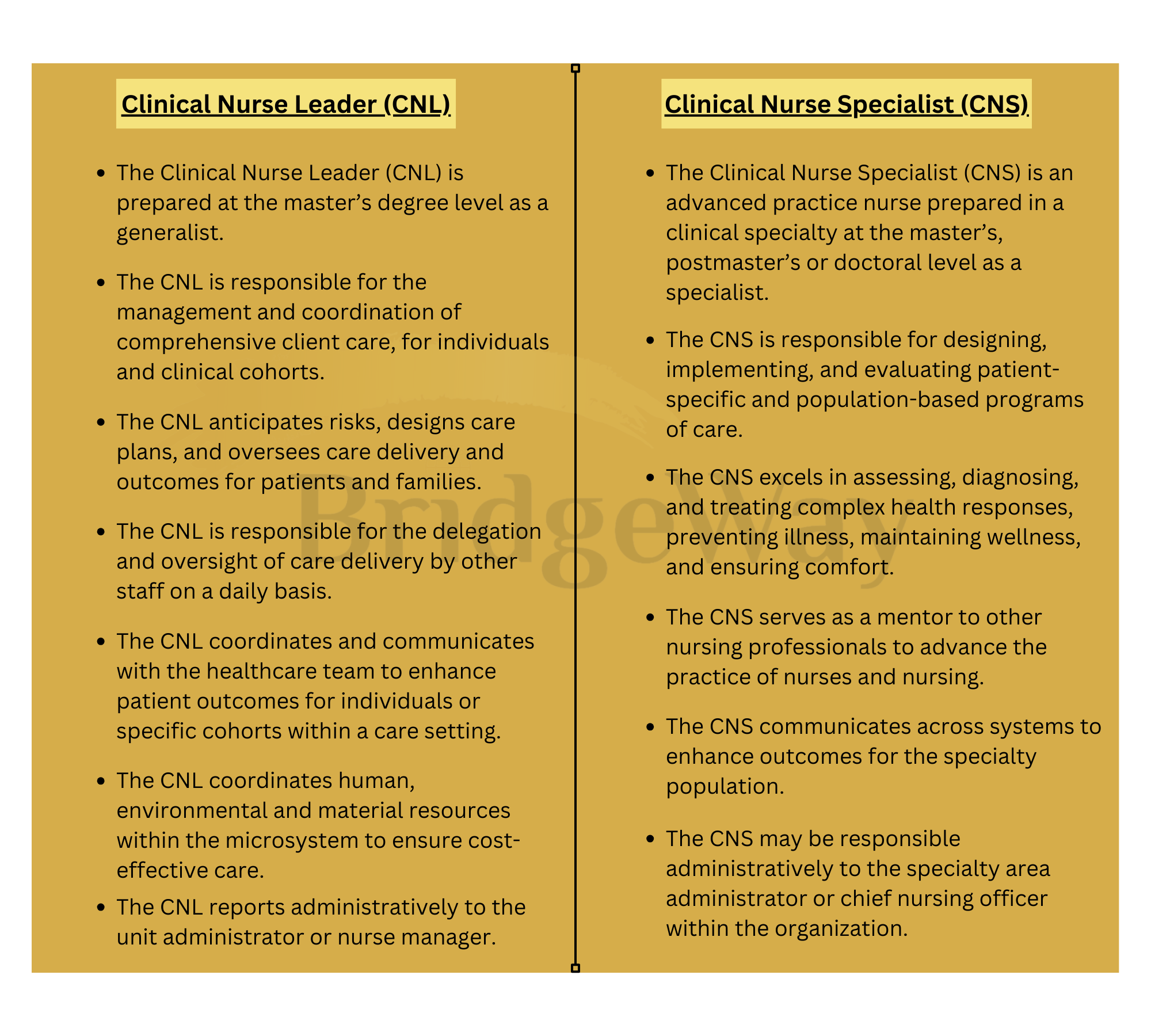
Comparing the Clinical Nurse Leader and Clinical Nurse Specialist Roles
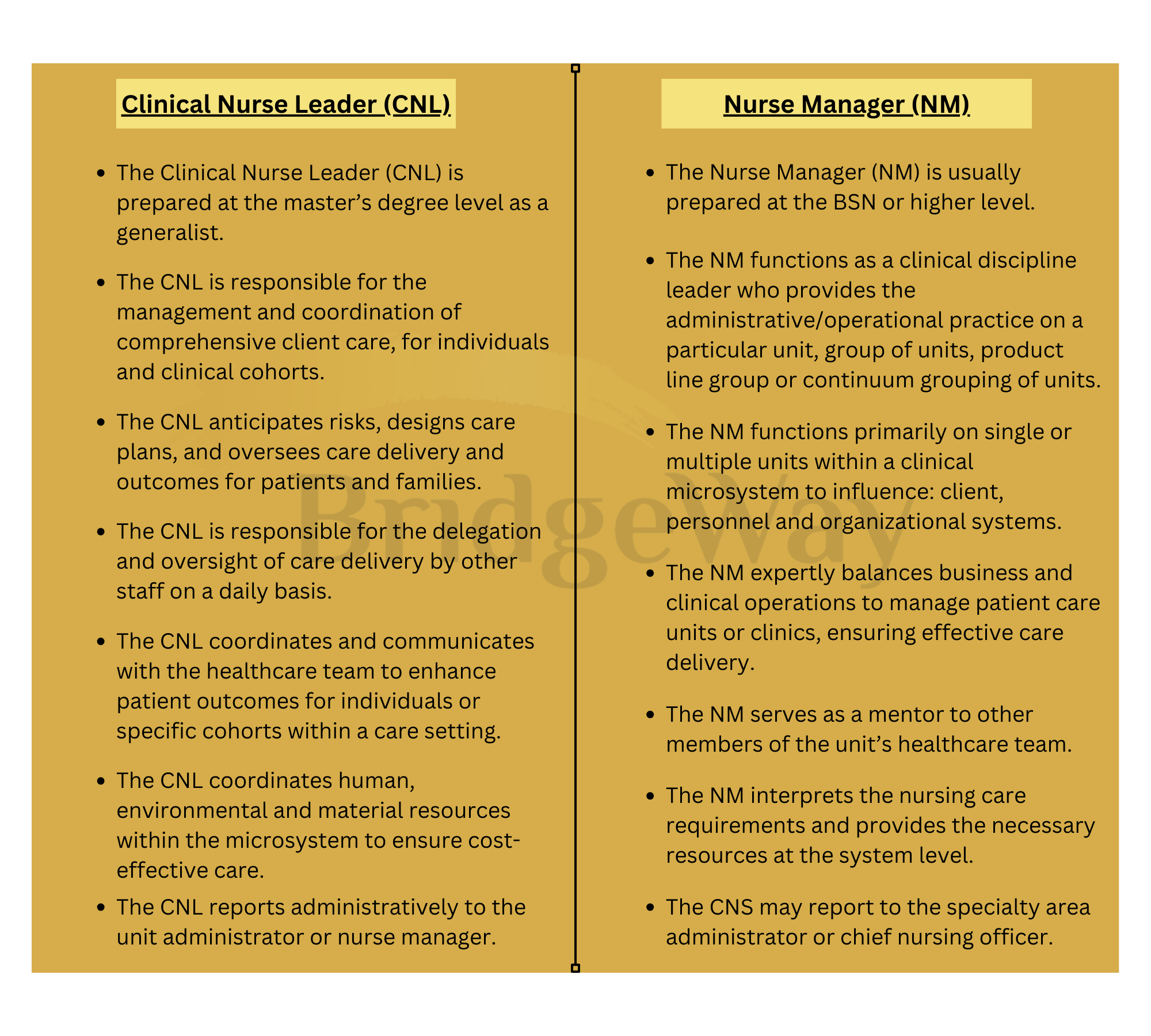
Comparing the Clinical Nurse Leader and Nurse Manager Roles
How to become a clinical nurse leader?
The Clinical Nurse Leader (CNL) is a nurse with a master's degree, trained to deliver care in diverse healthcare settings. Two types of programs are available;
Post-Master’s CNL Program
MSN Clinical Nurse Leader program
CNL graduates are well-prepared with the necessary graduate-level skills after completing their baccalaureate competencies. To ensure this, it is recommended that the CNL curriculum, including the clinical immersion experience, be completed within an 18-month timeframe. The exact duration may vary depending on the institution's academic calendar (semester or quarter system). Graduates of all master's degree CNL programs whether post-baccalaureate, RN-MSN, or second-degree are expected to achieve both the master's and CNL competencies.
Post-Master’s CNL Program
Post-master’s Clinical Nurse Leader (CNL) programs are designed for individuals who already hold a master's degree in nursing or a related field, preparing them for CNL practice and eligibility for the CNL certification exam. These students must successfully complete the graduate-level didactic and clinical requirements of a master’s CNL program through a formal certificate or master’s-level CNL program.
Post-master’s students are expected to achieve the same competencies as master’s CNL students, including the essential master’s core competencies and CNL-specific competencies. Additionally, coursework in pharmacotherapeutics, physiology/pathophysiology, and health assessment is required.
To gain hands-on experience in the CNL role, post-master’s students must complete a minimum of 300 hours in a supervised clinical immersion practicum. This practicum provides an opportunity to apply their knowledge in real-world settings under professional guidance.
Clinical/Practice Expectations for the Clinical Nurse Leader Program
The Clinical Nurse Leader (CNL) education program offers comprehensive didactic and clinical experiences to equip graduates with the necessary competencies. Faculty are responsible for evaluating the types of experiences, patient populations, and settings to ensure students develop the knowledge, skills, and abilities required for CNL practice across the healthcare continuum.
The curriculum should provide diverse opportunities for students to apply their learning in real-world settings. While the total clinical hours are determined by the program faculty, each CNL student must complete a minimum of 400 clinical/practice hours. Of these, at least 300 hours should be dedicated to an extended practice immersion experience, guided by an experienced CNL or other qualified professionals. This immersion experience is essential for integrating CNL practice into healthcare systems effectively.
The immersion experience allows students to refine their skills in a chosen healthcare setting, applying the competencies acquired throughout their education. It should take place in an environment that fully supports CNL practice and fosters strong interprofessional collaboration. Ideally, students should receive mentorship, either in person or virtually, from an experienced CNL. The immersion may occur in a single setting or multiple locations, depending on the student's needs. To maximize engagement with interprofessional teams and facilitate skill application, it is recommended that the immersion be structured over a 10- to 15-week period.
CNL Certification
Upon successfully completing a formal CNL education program, which includes a total of 400 practice hours, 300 of which are dedicated to CNL immersion, the graduate becomes eligible to take the CNL Certification Examination. This exam is administered by the Commission on Nurse Certification (CNC), an independent body of the AACN.
Students are encouraged to take the certification exam during their final term of a CNL master’s or post-master’s program or as soon as possible after graduation. For those taking the exam in their last term, program directors must confirm that all required clinical and immersion hours will be completed before graduation.
Graduates of entry-level or second-degree master’s programs that include CNL competencies may take the certification exam before sitting for the NCLEX-RN licensure exam. However, CNL certification will only be granted once the CNC receives proof of RN licensure.
How much does a clinical nurse leader make?
According to Indeed, the average annual salary for a Clinical Nurse Leader (CNL) is approximately $142,436 in the U.S with earnings ranging from $94,645 to $214,359 based on factors such as location, experience, and employer.
Government agencies, hospitals, and outpatient care centers offer some of the highest salaries for medical and health service managers, including CNLs. Starting your nursing career in USA as a Clinical Nurse Leader offers significant benefits because the employment opportunities for Clinical Nurse Leaders are expected to grow by 32% over the next decade, far exceeding the 4% average growth rate for all occupations.
Benefits of becoming a Clinical Nurse Leader
Career Advancement & Leadership Opportunities
Positions you as a leader within the healthcare team, improving patient outcomes.
Opens doors to higher-paying leadership and management roles.
Provides opportunities to mentor and support other nurses.
Competitive Salary & Job Growth
The average salary for CNLs is around $81,707 per year, with potential earnings exceeding $200,000 based on experience and location.
Job opportunities for CNLs are expected to grow by 32% over the next decade, significantly higher than the 4% average growth rate for all occupations.
Enhanced Patient Care & Safety
Leads quality improvement initiatives to enhance patient outcomes.
Reduces medical errors and promotes evidence-based practices in healthcare settings.
Improves patient-centered care through interdisciplinary collaboration.
Diverse Career Opportunities
CNLs can work in hospitals, outpatient facilities, government agencies, home healthcare, and academic institutions.
Offers flexibility in choosing specialties like geriatrics, pediatrics, oncology, or critical care.
Increased Professional Knowledge & Skills
Gains expertise in healthcare systems, informatics, policy, and leadership.
Develops skills in budgeting, strategic planning, and healthcare management.
Uses technology and data analytics to enhance healthcare delivery.
Contribution to Healthcare System Improvement
Plays a vital role in reducing healthcare disparities and improving equitable care.
Advocates for policy changes to improve patient outcomes and healthcare costs.
Leads initiatives that enhance safety, quality, and efficiency in healthcare.
Job Security & High Demand
CNLs are in high demand due to the increasing need for improved patient care coordination.
Their ability to bridge clinical expertise and leadership makes them valuable assets to healthcare organizations.
Professional Satisfaction & Impact
Provides a sense of fulfillment by improving healthcare systems and patient care.
Offers opportunities to educate, mentor, and empower future nurses.
Engages in lifelong learning through continuing education and certifications.
Becoming a Clinical Nurse Leader is an excellent career choice for those looking to advance in nursing, increase their earning potential, and make a lasting impact on patient care and the healthcare system.
Looking to Pursue a Master’s in Nursing in the USA with a Focus on Clinical Nurse Leadership?
At BridgeWay, we’re here to support your journey!
Our top-tier nursing programs are designed to equip nurses with advanced skills and compassionate care, meeting the rising demand for healthcare professionals.
We offer MSc Nursing scholarships in the USA, tailored for ambitious nurses eager to advance their careers. In the last three years, BridgeWay has granted scholarships to over 200 students.
Take a bold step toward a rewarding nursing career by enrolling in our MSN Clinical Nurse Leader program.
Apply today and turn your nursing aspirations into reality!